Breast Implant Revision
 According to the American Society for Aesthetic Plastic Surgery’s (ASAPS) annual statistics, more women choose to undergo breast augmentation every year. This surgery has become one of the most popular elective cosmetic procedures in the country and throughout the world. However, since breast augmentation remains a complex surgery, even a carefully planned and well-executed procedure may result in an unsatisfactory outcome. Fortunately, the majority of these cases can be corrected with breast implant revision.
According to the American Society for Aesthetic Plastic Surgery’s (ASAPS) annual statistics, more women choose to undergo breast augmentation every year. This surgery has become one of the most popular elective cosmetic procedures in the country and throughout the world. However, since breast augmentation remains a complex surgery, even a carefully planned and well-executed procedure may result in an unsatisfactory outcome. Fortunately, the majority of these cases can be corrected with breast implant revision.
- What Is Breast Implant Revision?
- Breast Implant Revision Consultation
- Reasons for Breast Implant Revision
- Breast Implant Revision Procedure
- Breast Implant Revision Risks
- Breast Implant Revision Recovery
- Breast Implant Revision Scars
- Breast Implant Revision Cost
What Is Breast Implant Revision?
Breast implant revision is a secondary procedure intended to correct problems from a previous breast augmentation. The surgery is similar to breast augmentation, but it is more complicated than the initial procedure. One of the challenges revision surgery poses is that the anatomy of the breast has already been altered from its natural state. This is why Dr. Neil J. Zemmel believes it is particularly important to choose a qualified plastic surgeon with extensive experience in primary breast augmentation, breast reconstruction, and breast implant revision to correct any irregularities and to achieve the size and shape you desire.
I was incredibly apprehensive to have my third breast surgery after 2 horrible experiences resulting in severe asymmetry and capsular contracture. Dr. Zemmel made me feel so comfortable because he was extremely thorough and very professional. He took time to answer any questions and made me feel confident in my decision to do a third surgery 4 years after my initial 2. I am beyond thrilled with my results. I feel great again and my breasts look amazing! My only regret is that I did not do this sooner! Thank you to Dr. Zemmel and his outstanding staff, love them all!
Emily S
August 10, 2016
What Does the Breast Implant Revision Consultation Involve?
During your breast revision consultation, Dr. Zemmel will listen to your reasons for wanting revision surgery, discuss the details of your past breast procedure(s), and perform a physical examination. In addition to this exam, precise measurements of the breast and chest wall, and custom-tailored implant selection, Dr. Zemmel will evaluate your medical records directly pertaining to your previous breast augmentation to design a treatment plan that can respond to your reason for seeking breast implant revision. Additional imaging tests may be needed to detect if a rupture has occurred.
When planning breast implant revision, your surgeon will take into account changes that have occurred to the breasts over time. They include thinning of the breast skin and breast tissue, thickened breast implant capsules (capsular contracture), breast shape abnormalities and sagging (ptosis), implant rupture, and scar tissue. Dr. Zemmel will also use any paperwork or other information you may have from the initial procedure to plan your implant revision.
With all of this information, Dr. Zemmel will be able to plan the specifics of your revision procedure, helping you understand what the process will entail and the type of results you can realistically expect.
What Are Common Reasons for Breast Implant Revision Surgery?
The vast majority of breast augmentation patients are very satisfied with their results. However, breast augmentation does not stop the breasts from changing shape or consistency over many years’ time. There are also a number of cosmetic concerns that can result from an initial breast augmentation. If you are unhappy with your implant shape or implant size, you do not need to remain unsatisfied. It is possible to further modify the shape of your breasts with a revision procedure.
Dr. Zemmel specializes in complex revisional surgery of the breasts. He has a strong professional and intellectual interest in complex, challenging surgeries and will make every effort to address your unique needs.
With a revisional procedure, Dr. Zemmel can correct most of the reasons women are typically unhappy with their initial results. By directly addressing – and correcting – the following conditions, Dr. Zemmel can provide you with beautiful breasts that both look and feel natural.
- Capsular Contracture
- Silicone Implant Rupture
- Saline Implant Deflation
- Asymmetric Breast Implants
- Breast Implant Rippling
- Implant Size Issues and Post-Operative Size Regret
Capsular Contracture
All medical grade implants, whether they are breast implants, replacement joints, suture material, or plates and screws used in orthopedic surgery, are made of artificial materials. The materials used such as silicone, titanium and vanadium are biocompatible, meaning that your body will incorporate the prosthetic and, over time, tolerate the artificial material. Your body knows that the material is “not self” and will form a thin layer of tissue around the prosthetic. This serves as the interface between the tissue of your body and the prosthetic.
A breast implant is made from artificial materials, mainly silicone, just like any other prosthetic. During breast augmentation, a silicone or saline implant is inserted and the body begins to heal around the implant during recovery. This process takes approximately 2 to 4 weeks. In most cases, a thin layer of soft tissue, referred to as the capsule, surrounds the implant.
In the majority of patients (greater than 98%) the capsule remains thin, soft, pliable, and essentially undetectable. However, in approximately 1% to 2% of patients, this capsule can thicken, harden, and distort the initial shape of the implant. Capsular contracture can manifest in varying degrees of severity, and can alter the intended shape and position of the implant or cause undue stress to the overlying skin.
What Causes Capsular Contracture?
The current theory regarding the cause of capsular contracture is that a small amount of contamination is introduced during surgery. The amount of contamination is small and not enough to cause a robust infection demonstrated by fever, severe redness, swelling, and pain. The small amount of contamination is enough, however, to cause an inflammatory response around the implant. This incites the production of a thicker capsule and ultimately causes capsular contracture.
Dr. Zemmel takes every precaution possible in surgery to ensure that the risk of contamination is close to zero and, therefore, the risk of capsular contracture minimized.
How Does Dr. Zemmel Work to Prevent Capsular Contracture?
- Dr. Zemmel is the only member of the operating room team to touch and handle the implants. In many cases, a Keller funnel is utilized to perform a “no-touch” implant placement, which also helps minimize the risk of a low-grade infection known as biofilm.
- Dr. Zemmel changes gloves a minimum of 3 times during surgery to ensure the highest levels of sterility.
- Dr. Zemmel washes the implants and implant pockets with three different antibiotics: vancomycin, gentimycin, and ancef.
- All of Dr. Zemmel’s patients receive pre-operative and post-operative antibiotics.
- Dr. Zemmel performs all breast implant surgeries in the main operating rooms of an accredited hospital. By using the main operating rooms of an accredited hospital, he has access to the best equipment and the highest levels of sterility.
- Dr. Zemmel places both silicone and saline implants in the submuscular position, which has a significantly lower chance of developing capsular contracture than the subglandular position.
The reoperation rate for capsular contracture in Dr. Zemmel’s primary breast augmentation practice is less than 0.5%.
Baker System for Grading Capsular Contracture
Capsular contracture is graded according to the severity of the hardness, tenderness, and distortion of the breast shape. The Baker grading system is used:
- Grade I: The breast appears natural in size and shape, and is soft
- Grade II: The breast is slightly firm, but is non-tender, and appears natural in shape
- Grade III: The breast is firm and shows some distortion of shape
- Grade IV: The breast is hard, tender to the touch, and shows obvious distortion of shape
How Is Capsular Contracture Treated?
To correct cases of Grade III/IV capsular contracture, surgery is typically required. The compromised implant is typically removed and replaced with a new implant. In addition, Dr. Zemmel will either perform a capsulotomy (opening of the capsule) or a capsulectomy (removal of the capsule), or a combination of the two.
If a capsulectomy is required, Dr. Zemmel prefers to use the en bloc removal technique whenever it is safe to do so. This involves removing the entire capsule with the implant still inside. By using this technique, Dr. Zemmel can remove a potentially damaged implant and any leaked material at once. He does this by carefully separating the capsule from the surrounding tissue and removing it through a tiny incision. If the capsule will not fit through the incision with the implant intact, the contents of the capsule may need to be emptied prior to removal. While our surgeon strives to perform a capsulectomy via en bloc, he will ultimately choose the technique with the least risk, which often cannot be decided until the time of surgery.
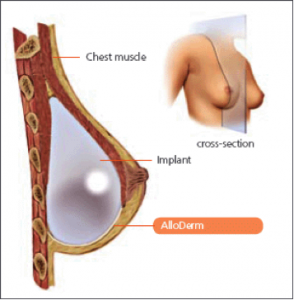
If your original implants are placed in the subglandular position (on top of the muscle), your surgeon may offer you a pocket reassignment procedure. This includes placing your new implants under the pectoralis muscle and suturing closed the previous subglandular pocket. This places your new implants in a completely new pocket under the muscle, ultimately giving your new implants an undistributed, fresh environment to heal within.
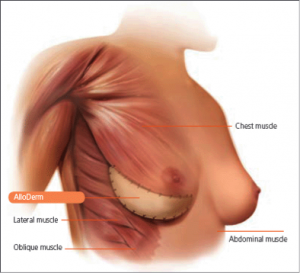
Your surgeon may also offer the use of acellular dermal matrix (ACDM or Alloderm®) for capsular contracture repair. There are excellent studies showing that the use of acellular dermal matrix implanted within the breast pocket interrupts the reformation of capsular contracture. While the mechanism of action is still under investigation, Dr. Zemmel has used this technique in a significant number of revision patients with excellent success.
If the patient has a previous periareolar incision or an inframammary incision, the old incision may be used for this revision. A transaxillary incision cannot be used for this type of revision and therefore a new incision will be made.
Some patients elect to switch from saline to silicone implants during breast implant revision surgery for capsular contracture in order to further reduce the chance of recurrent contracture and to improve the overall texture of the breasts. During the breast surgery consultation process, your surgeon will review all of your available options and explain which approach to correcting capsular contracture he recommends for your individual circumstances.
In summary, Dr. Zemmel uses the following techniques to treat and repair capsular contracture:
- Implant exchange
- Switching from saline to silicone implants
- Capsulectomy (using the en bloc technique when possible)
- Capsulotomy
- Placement of acellular dermal matrix
- Pocket reassignment
Silicone Implant Rupture
Unfortunately, no prosthetic implant can last a lifetime. As with all man-made parts, prosthetic implants have a lifespan and will need to be replaced. Though modern breast implants are designed for extreme safety and durability, the lifetime of previous generation breast implants from the 1970s and early 1980s had higher rupture rates. These implants had thinner, single-layer implant shells and a liquid silicone filler. Women who have silicone implants placed during this era have essentially a 100% chance of rupture today. Women who have rupture may have silicone gel contained only within the breast pocket, or may have gel that has migrated out of the original pocket. This is called extracapsular gel.
Silicone gel has been shown NOT to cause systemic illnesses such as arthritis, autoimmune disease, and irritable bowel syndrome. The extracapsular gel can cause local areas of hard scar tissue called granulomas, which can alter the texture of the breast and potentially obscure mammography.
For these reasons, Dr. Zemmel recommends all women with breast implants placed during this time period undergo an evaluation for possible rupture. During your initial consultation, your surgeon will perform a complete history and physical examination, focusing on the breast exam. He may then recommend an imaging test of the breast to examine the possibility and degree of the rupture.
Modern silicone implants such as the Mentor MemoryGel® implant have a significantly lower rupture rate. This is due to a redesign of the implant. Current implants have a multilaminar shell and are filled with cohesive silicone gel. The long-chained silicone molecules are more cross-linked, giving the gel a thicker consistency. Therefore in the event of a rupture, silicone gel should not migrate out of the original breast pocket. In fact, you can cut these implants in half and the silicone gel stays in place.
The rupture rate for modern cohesive gel implants is approximately 1%, six years after implantation. Because the gel is cohesive, no shape change will occur and patients typically do not experience any negative symptoms. These implants are said to rupture “silently.” Since these ruptures can be so difficult to detect, the FDA recommends patients with silicone implants schedule periodic MRIs to monitor for rupture. Your surgeon will guide you through this process.
Breast Implant Exchange for Silicone Rupture
If a rupture is detected, your surgeon will likely advise replacement of the implants. To correct a silicone implant rupture, Dr. Zemmel will replace the compromised implant with a new one. He always replaces both implants at the same time to reset the lifespan of both implants. In doing so, both implants will have the benefit of being made from the strongest and most advanced materials available, reducing the likelihood of a future rupture. In some cases, this implant replacement is covered by a manufacturer’s warranty.
Please note: If you are outside of the warranty period for your silicone implants and you have a rupture, your health insurance plan may cover the removal portion of the procedure.
Most commercial insurance plans and Medicare cover the removal of ruptured silicone implants, even if they were originally placed for cosmetic purposes. The coverage includes removal of the ruptured implants and removal of silicone material outside of the implant if necessary. Replacement of the new implants is not covered and is considered cosmetic by all insurance carriers. Our surgeon and team will guide you through the process of obtaining insurance approval.
The surgery for replacing older generation and newer generation ruptured silicone implants requires a number of complex steps. These can include:
- Using your previous inframammary or periareolar incision to gain access to the original breast pocket.
- Total capsulectomy to completely remove the previous breast implant capsule.
- Removal of the previous implant shell and any implant filler material.
- Removal of extracapsular gel and any silicone granulomas.
- Pocket reassignment to the submuscular position if necessary.
- Closure of the previous subglandular pocket.
- Placement of acellular dermal matrix (ACMD) to augment the lower portion of the breast and stabilize the implant pocket.
- Sizing and placement of new implants.
- Mastopexy (breast lift) as necessary.
Your surgeon will review all of your available options during the initial consultation.
Saline Implant Deflation
Unlike a silicone implant rupture, a saline implant rupture is often immediately noticeable and results in the deflation of the outer implant shell. When a saline implant is ruptured, the saline solution exits the silicone shell and is absorbed by the body. This is a harmless process.
Some patients will experience a rapid deflation over 24 to 48 hours’ time. This is usually due to a rupture of the implant shell, which causes saline to rapidly leak. Other patients may experience a slower, intermittent leak over several weeks’ time, which is usually caused by failure of the fill valve.
Newer generation saline implants have a rupture rate of 1.8% per year.
Breast Implant Exchange for Saline Deflation
To correct a saline implant rupture, the compromised implant will be replaced with a new one. Dr. Zemmel typically recommends that patients replace both implants during the same procedure to reset each implant to the same lifespan. Some patients with saline implants opt to switch to silicone implants at this time to improve the texture and feel of the implants.
Dr. Zemmel also strongly recommends replacing the implants with 2 weeks of rupture. After this time, patients with ruptured saline implants risk the breast pocket collapsing around the ruptured implant shell. This makes surgery more difficult as the pockets must be reopened (capsulotomy) to the new implant.
The surgery to replace saline implants, when performed in a timely fashion, is usually less invasive than the original breast augmentation surgery. The steps required for replacement are:
- Reopening the old periareolar or inframammary incision, or creating a new incision in this area if a previous transaxillary incision was used.
- Removal of the ruptured implants.
- Reopening the upper and medial portion of the breast pocket capsule.
- Reinsertion of the new implants and filling them with saline.
- Closure of the incisions.
Asymmetric Breast Implants
Greater than 95% of women have measurable, natural asymmetry of the breasts.
Many factors influence the size and shape of the breasts, including:
- The quality and quantity of your breast skin.
- The presence of stretch marks.
- The amount and distribution of breast tissue within the breast.
- The size and position of the nipple and areola on the breast.
- The position, shape, and tightness of the crease of the breast (inframammary fold).
- The shape of the ribs.
- The shape and width of the breast bone.
- The shape and position of the pectoralis muscles.
Dr. Zemmel is able to surgically alter some of the above variables, but some elements contributing to asymmetry cannot be altered, such as the shape of your bone structure. Dr. Zemmel believes that some asymmetry between the breasts before and after surgery is both normal and natural. Your breasts are as individual to you as is your face and your fingerprints.
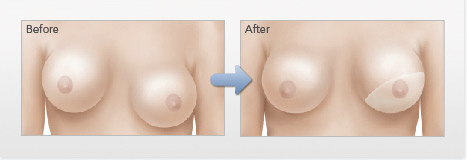
There are some women, however, who do experience a degree of asymmetry after surgery that is unnatural and gives the breasts a displeasing shape and contour. Occasionally, the asymmetry is present immediately after the initial procedure. In other situations, a woman may experience progressive asymmetry over time as the breast ages. Dr. Zemmel can address both scenarios.
How Is Breast Implant Asymmetry Treated?
To improve symmetry after breast augmentation, your surgeon can perform a number of techniques in surgery, depending on the factors contributing to the asymmetry, including:
- Breast implant exchange and resizing, if necessary.
- Repositioning the breast implant with capsulotomy (opening of the breast pocket).
- Repositioning the breast implant with capsulectomy (removal of breast pocket capsule).
- Repositioning the breast implant with capsulorrhaphy (suturing closed part of the breast pocket).
- Pocket reassignment as necessary.
- Placement of acellular dermal matrix as necessary to reinforce the pocket repairs.
- Breast lifting (mastopexy) as necessary to remove excess breast skin and reposition the nipple and areola higher on the breast.
Implant Malposition
For most women, the ideal position for an implant is directly beneath the breast. Additionally, most women desire the nipple and areola to be centrally located over the area of the breast with the highest degree of forward projection. When an implant shifts after breast augmentation, this ideal position is lost and may require repositioning of the implant for optimal correction. Dr. Zemmel uses a combination of techniques to achieve this, depending on your particular circumstances. By incorporating AlloDerm® (an acellular dermal matrix) into the revision, he can reinforce capsule repairs by strengthening the tissue surrounding the implant while also minimizing the chances of capsular contracture. There are four main categories of implant malposition:
- Medial Subluxation and Symmastia: Symmastia is a condition characterized by the extreme narrowing or complete elimination of the cleavage between the breasts. Creating too medial of a breast pocket causes this condition. The medial or inner border of the pectoralis major muscle was completely released, allowing the implant to migrate across the chest. In the case of subglandular implants, the subglandular pockets merge across the breastbone. In severe cases, the right and left breast pockets cross the breastbone centrally to form one continuous pocket across the chest. The right and left breast pockets form one larger pocket containing both implants. This gives the appearance of one large single breast. The slang term for this condition is “uniboob.” To correct symmastia, our surgeon can recreate cleavage and the natural separation of the breast pockets via a number of techniques. The state-of-the-art surgical technique is to recreate the inner aspect of the breast pocket with sutures (capsulorrhaphy). This repair is then reinforced with acellular dermal matrix (Alloderm®). This creates a barrier across the breastbone and separates the right and left breast pockets. If the implants are located in the subglandular position, a pocket reassignment may be necessary.
- Lateral Subluxation and Malposition: Conversely, when the breast pockets are placed too far apart, the implants can laterally displace and migrate to the outer side of the chest wall. In extreme cases, patients may experience migration of the implants towards the underarms when lying down. This typically occurs if the lateral (outer) aspects of the implant pockets are opened too far laterally initially during surgery. It can also occur over time as the augmented breast ages and the implant pockets stretch. To correct lateral subluxation and malposition, Dr. Zemmel can use a doubly-reinforced suture line (capsulorrhaphy) to close the lateral aspect of the pocket and further reinforce it with acellular dermal matrix (Alloderm®). This will effectively move the implant centrally across the chest wall and improve cleavage. Occasionally, a slightly smaller implant is needed.
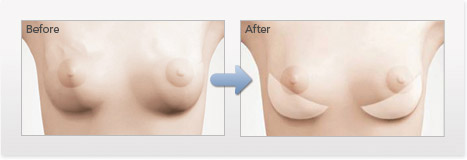
- Inferior Malposition (“Bottoming Out”): Inferior malposition occurs when an implant settles abnormally low on the chest wall after breast augmentation. Also known as “bottoming out,” this condition can also cause the nipple and areola to appear higher on the breast than intended. This can occur initially during surgery if the inframammary fold is abnormally lowered or over a period of time as the breast pocket stretches. To correct inferior malposition, your surgeon can raise the level of the inframammary crease to elevate the implant to its proper position. This is done similarly to lateral and medial subluxation with the use of a double-layered suture repair of the inframammary fold (capsulorrhaphy) reinforced with acellular dermal matrix.
- Superior Malposition: If an implant fails to settle after an initial breast augmentation, the implant can remain higher on the chest wall than intended. This is usually caused by incomplete release of the lower border of the pectoralis muscle during the initial surgery. The repair for this condition consists of re-entering the breast and releasing the remainder of the muscle to reposition the implant.
If this condition is progressive over time, and the implant becomes firm, then capsular contracture may be the cause, and your surgeon will discuss this type of repair at length as outlined above.
Breast Implant Rippling
Rippling occurs when the folds or waves of an implant become visible through the breast tissue and skin. If you have thin skin around the breast or a minimal amount of breast tissue, you may be at a higher risk for implant rippling. Saline implants are known to be more susceptible to rippling than silicone implants, and are particularly prone to rippling when under-filled. In addition, submuscular implants (placed under the muscle) have a lower risk of rippling than subglandular implants (placed over the muscle). As a general principle, the more tissue you bury an implant under, the less likely you will see and feel the implant. The thinner the patient, the greater the chance there is of seeing and feeling the implants. This holds true for both saline- and silicone-filled implants. The thicker the soft tissue covering the implant, the less likely a patient will see and feel rippling.
How to Prevent Breast Implant Rippling
When performing a primary (or first-time) breast augmentation, Dr. Zemmel performs a number of maneuvers in surgery to reduce the risk of rippling.
- Implants are always placed in the submuscular or dual plane position to bury the implants under a thick layer of tissue.
- In very thin patients, silicone implants may be strongly recommended.
- When using saline implants, our surgeon will fill each implant to its maximum fill volume, or slightly overfill the implants to smooth out the implant edges
Typically, rippling is evident in the lower outer and lower inner quadrants of the breasts. This occurs where the soft tissue covering of the breast is thinnest. Often, patients will demonstrate rippling by leaning over, which exacerbates the effect.
When performing revision breast augmentation, Dr. Zemmel may improve or eliminate rippling altogether by the following techniques:
- Conversion of saline implants to silicone implants.
- Pocket reassignment from the subglandular to submuscular position.
- Reinforcement and thickening of the rippling areas with acellular dermal matrix (Alloderm®).
- Autologous tissue fat transfer (fat grafting) to thicken soft tissue.
Implant Size Issues and Post-Operative Size Regret
Rarely, a woman who undergoes breast augmentation decides she would like to change the size of her implants. At Richmond Aesthetic Surgery, Dr. Zemmel makes every effort during your pre-operative evaluation to measure and size your implants in order to reduce the chance of a future size change. He will take over 20 measurements of the breasts. You will then discuss saline versus silicone implants and medium and high-profile shaped implants. Finally you will try on a number of implants and examine yourself in the mirror to select the perfect fit. You will have at least 2 fittings with your surgeon before surgery to choose your implant size.
Dr. Zemmel will personally guide you in choosing the perfect implant size. He believes in a natural, proportional, and balanced breast augmentation. A balanced breast augmentation will re-proportion your upper and lower body. This will accentuate your waistline and further add to your results.
After seeing their final results, some women feel they have made the wrong implant selection for their breast augmentation. The most common regret after surgery is that women wish they went with a larger implant. Occasionally a woman may feel she chose too large of an implant. Dr. Zemmel believes in spending more time during your initial consultation and pre-op visit trying on implants in order to “get it right” this first time. This extra time spent trying on different implant sizes reduces the risk of post-operative size regret. At Richmond Aesthetic Surgery, our surgeon’s revision rate for post-operative size regret in their primary breast augmentation patients is approximately 0.70%.
If you decide to change the size of your implants, the exchange procedure is less invasive than your original surgery, with little downtime. During the consultation process, your surgeon will perform a physical examination, listen to your aesthetic concerns, and make recommendations for an implant size that can create a proportionate, balanced, and natural look. For patients seeking larger implants, Dr. Zemmel cautions against sizes that are extremely large in relation to your figure, as this will increase your risk for complications. When switching implants for a smaller size, Dr. Zemmel carefully plans the surgical approach to help safeguard against deflation or sagging of the breast. In some cases, a breast lift may be needed when decreasing the size of your implant to maintain a more youthful breast shape.
What Does the Breast Implant Revision Procedure Involve?
Primary breast augmentation is a complex operation that must be performed by a plastic surgeon. Revision implant surgery is an order of magnitude more complex since the patient’s natural anatomy has already been altered. Additional challenges, such as thinning breast tissue, ruptured implant material, and scar tissue, make breast implant revision a complicated procedure requiring exceptional skill and experience. We recommend that you seek out a plastic surgeon with extensive experience in complex breast revision and reconstruction.
Due to the intricate nature of breast implant revision surgery, every detail of the procedure must be highly customized to each patient and their unique concerns and aesthetic goals. Dr. Zemmel’s approach to revision surgery uses many of the same breast surgery techniques as the augmentation procedure, but also incorporates techniques used in breast reconstruction for breast cancer.
In many cases, your surgeon will be able to perform your revision through the same incisions as your initial breast augmentation. Depending on the reason for your revision, you may undergo breast implant removal using the capsulectomy en bloc or capsulotomy technique. If you are receiving new breast implants, you may be recommended to switch to a different implant type and/or utilize the submuscular approach. Acellular dermal matrix may be needed to reinforce the breast pocket. If you have excess skin or are switching to a smaller implant size, breast lifting may be necessary to achieve the most aesthetic outcome.
All of these details and more will be discussed with you during your consultation, at which point you are encouraged to ask questions and express any concerns. Together, you and your plastic surgeon can design a treatment plan that can help you achieve your desired look.
What Are the Risks of Breast Implant Revision Surgery?
Dr. Zemmel’s primary goal is to give patients the safest and most reliable outcome. His top priority is patient safety. Therefore Dr. Zemmel and the entire team at Richmond Aesthetic Surgery take a number of precautions when performing breast implant revision surgery to maximize patient safety including:
- Performing surgery only in the main operating rooms of fully accredited hospitals.
- Performing surgery only using board-certified anesthesiologists and nurse anesthetists.
- Performing surgery with the same operating room team for 8+ years.
- Using the highest-quality instruments, implants, and suture materials available.
- Closely monitoring all patients during every phase of recovery.
The general risks of breast implant revision surgery are very similar to those of breast augmentation surgery. Bleeding, infection, implant rupture, and alteration in nipple sensation are rare, but possible issues.
Revisional surgery is by nature more complex, more difficult, and less predictable. Therefore, some degree of natural post-operation asymmetry is to be expected. Because implants are measured in ccs (milliliters), a post-operative cup size cannot be guaranteed. Furthermore, there is no uniform sizing for bra size, and every bra manufacturer has a different fit. In patients with already existing capsular contracture, there is an elevated risk for having a recurrent contracture. When treating rippling, some patients may experience significant improvement, but not complete resolution of rippling.
With that in mind, Dr. Zemmel takes special care during the pre-operative planning stage to address all of your aesthetic concerns, and he can create results that make you feel more youthful, beautiful, and rejuvenated. By following the detailed pre-operative and post-operative instructions provided by your surgeon during the consultation process, you can greatly reduce the risk of complications.
What Can I Expect from My Breast Implant Revision Recovery?
Dr. Zemmel’s top priorities for breast implant revision procedures are safety, comfort, and achieving cosmetic results that will correct any dissatisfaction resulting from your initial breast augmentation. The recovery and healing process for breast implant revisions are similar to breast augmentation and breast lift surgery, and in many cases is lessened. Your surgeon will meet with you frequently over the first month of your recovery to monitor your progress. As with your initial breast augmentation, there will be some limitations on your physical activity for the first few weeks.
After the second week of your recovery, Dr. Zemmel recommends that you begin a scar treatment regime to minimize the long-term appearance of any incisions. Though you will be able to notice results shortly after your surgery, the final outcome of your breast implant revision may not be fully evident until 6-12 months post-op. During this time, the body will continue to heal and you should see your results constantly improving.
Our plastic surgeon and his knowledgeable team are available to you at any time throughout your recovery. Please visit our office or contact us by phone if you have any questions or concerns during the course of your recovery. Dr. Zemmel believes the meticulous post-operative care we provide to our patients at Richmond Aesthetic Surgery is an essential component to achieving the beautiful look they desire.
What Will My Breast Implant Revision Scars Look Like?
The scars from breast implant revision surgery are typically very similar to those from a primary breast augmentation. This is because revisional surgery can often be performed through the existing scars. If you have prominent scarring from your initial breast augmentation, this can also be improved during your implant revision procedure. During your consultation, your plastic surgeon can provide you with a more realistic expectation as to what you can expect with your post-operative scars.
How Much Does Breast Implant Revision Cost?
The cost of a breast implant revision will greatly vary based on the complexity of the procedure, location of the practice, expertise of the surgeon, and any associated fees. A breast implant revision may start around $9,000 or cost up to about $12,000. Once a treatment plan has been customized to your needs, our team will provide you with a personalized cost quote, including the different fees involved with your procedure. Unfortunately, health insurance typically does not cover the cost of breast implant revision since it is considered a cosmetic procedure. If you would like to learn about our breast augmentation financing options, our staff would be happy to help you get started.
Will My Breast Implant Warranty Cover My Revision Surgery?
In some cases, the cost of breast implant revision surgery may be covered under your implant warranty. Breast implant manufacturers often provide warranties that cover common problems, such as implant rupture, or offer financial assistance for specific complications, like capsular contracture. For more information, visit our surgeon’s guide to breast implant warranties. Your surgeon will discuss your warranty coverage at length with you during your initial consultation. Please bring any paperwork related to your original surgery with you to your consultation.
Contact Us
If you would like to learn more about how Dr. Zemmel can help you address your cosmetic concerns regarding a previous breast augmentation with revision surgery, please contact our office today.



